In part one of this blog series, we answered common questions posed by medical directors and claims management leaders at health plans. Because accurately reviewing and identifying genetic testing claims payments can be incredibly complex, we continue the conversation with our experts in this blog and turn our focus to the logistics of the payment integrity process.
Q: Our claims system is overwhelmed by the new genetic tests that are released every month, as well as new CPT codes. How can we stay current on these? If we choose a genetics services vendor to help us, how can we be sure they’re staying abreast of test and code changes?
A: CPT codes for genetic testing are constantly changing, making it challenging for claims systems to remain accurate. As codes are released, changes in laboratory billing practices are inevitable. In order to stay abreast of changes, it is critical to have a team that can accurately interpret the impact of those changes and ensure claims are being coded appropriately.
To do this, your team needs to have specific, high-level genetics expertise. Evaluating CPT codes in the genetics space is complex and requires a very different knowledge base than evaluating other types of CPT codes. Genetic counselors, especially ones with experience in the laboratory, are uniquely skilled and can be a great asset in managing these changes. Coding changes should be monitored at least quarterly and cross-referenced against current practices to adjust for impact on laboratory billing practices. This requires not only the knowledge base but also systematic processes and procedures to ensure the proper maintenance of codes and assessment of downstream impact.
Our clinical team constantly monitors best practice standards, guidelines, and changes in CPT coding for how they are impacting genetic testing utilization. We assess which approach to apply. Sometimes the solution is a new edit or enhancing a current edit. Sometimes, it might be a change to policy or an adjustment to prior authorization requirements. There isn’t a one-size-fits-all solution for managing genetic testing. Each new development requires expert analysis to determine the proper solution for each test and indication. This collaborative approach allows plans to be proactive vs. reactive – genetic testing management is not something that is a set-it-and-forget activity.
Q: How would a genetic test payment integrity solution be integrated into our current claims system? How would updates be received and implemented? What is required on our part?
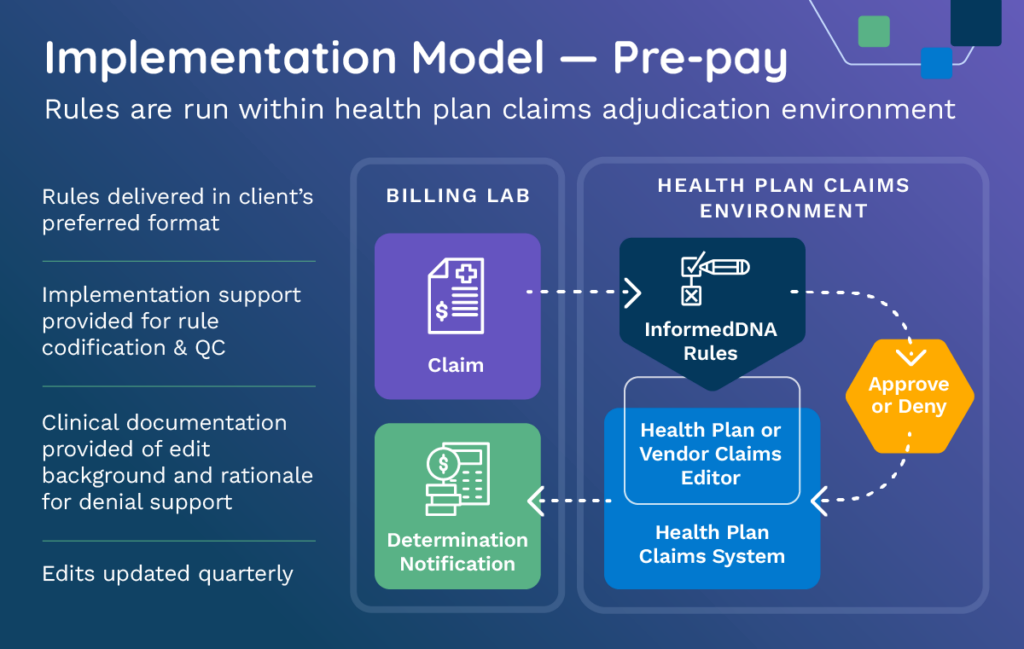
A: In the pre-pay environment, our edits can be housed in the health plan’s own claims adjudication environment or accessed through a claims editing system via one of our vendor partners. The claim is adjudicated against expert edits for a recommended determination and that determination is applied based on the health plan’s standard industry procedures.
InformedDNA supplies rules in the client’s preferred format and works with the plan during the implementation process, providing codification and QC support. All edits come with customized documentation of the background and rationale to support the action. Appeal support is also available.
In the post-pay environment, the health plan sends historical claims data to us for expert analysis. This process includes:
- Analysis against proprietary algorithms, based upon genetics expert review of health plan policy
- Batch analysis and return of results, outlining recommended denials, recovery amounts, and support for denials
After this, the health plan or vendor partner proceeds with recoveries. The images below show the difference between the pre-pay and post-pay environments:
Implementation Model – Pre-pay
Implementation Model Pre- or Post-pay
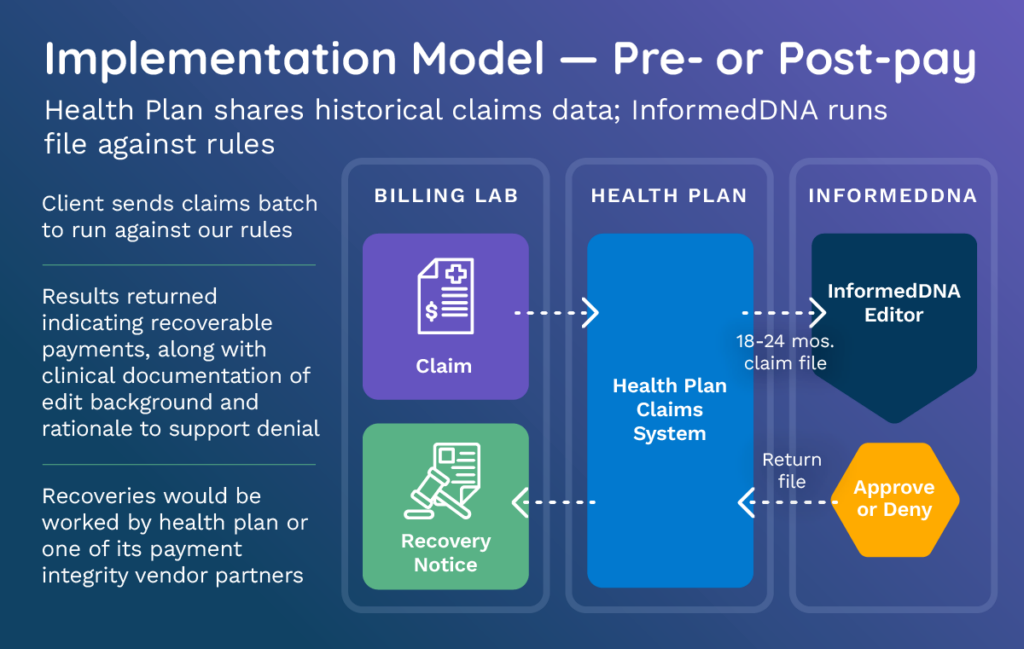
We provide updates on a quarterly basis regardless of how the solution is implemented. If working with a vendor partner or providing batch claims, edit updates are incorporated as soon as they are available without any work required from the health plan. When edits are licensed by the plan, any edit adjustments or enhancements need to be made by the health plan edit codification team.
Q: How do we know if our plan is operating as it should? How can we tell if our spending is in line with industry norms?
A: Because genetic test spending and the policies to manage that spending vary widely across health plans, it can be challenging to know how your solution is stacking up in comparison to industry-wide benchmarks.
Some health plans might have higher genetic testing spending as a direct result of policies or biomarker legislation that allow for broader coverage of genetic tests compared to other health plans. It could also be that health plans have higher genetic testing spending because they haven’t mastered the right combination of prior authorization and claims edits to enforce their existing policies. The variability across health plans is significant and looking at genetic testing spending alone is not sufficient to identify appropriate solutions.
As health plans struggle to find the right balance between genetic testing coverage and spending, a full-cycle approach to Genetic Benefits Management is critical. InformedDNA enables health plans to stay ahead of the curve by augmenting a plan’s in-house team with comprehensive clinical genetics expertise, including pre- and post-test services.
An evaluation and analysis will help determine where the plan’s gaps exist and which solutions are best positioned to solve any problems. We empower health plans to promote precision medicine, optimize spending, and avoid unnecessary and unpleasant experiences for members and providers through solutions that are appropriately targeted to meet the unique needs of each health plan.
InformedDNA can determine the savings potential of a genetic testing payment integrity solution for your organization at no cost. We’ll perform detailed claims analyses to identify instances of overpayment-and estimate how much your plan could save from our solutions. The process is simple:
- We’ll schedule a brief meeting with you to gather information about your plan and its genetic test claims challenges.
- We’ll then send you our Claims Data Submission Spec that details the data we’ll need in order to perform a savings analysis.
- After receiving your data, we’ll perform the analysis which will summarize your genetic testing spend trends and potential for savings utilizing our payment integrity products. This process takes approximately 2-3 weeks.
- We’ll set up a meeting with your team and ours to share the analysis results and answer any questions you have.
Contact us today for a complimentary savings analysis
With the nation’s largest and most experienced staff of lab-independent genetics specialists, InformedDNA enables health plans to stay ahead of the curve by augmenting a plan’s in-house team with comprehensive clinical genetics expertise, including pre- and post-test services. We empower health plans to promote precision medicine, optimize spending, and avoid unnecessary and unpleasant experiences for members and providers.
To learn more about our services, click here to submit a brief form and we’ll get back to you right away. Or, give us a call at 844-846-3763.


